Understanding Tardive Dyskinesia: Symptoms, Side Effects, and Treatment Options
Tardive dyskinesia (TD) is a neurological disorder characterized by involuntary, repetitive movements of the face, tongue, and other body parts. This condition often develops as a side effect of long-term use of certain medications, particularly antipsychotics. As awareness of TD grows, it's crucial to understand its symptoms, potential dangers, and available treatment options.
What are the common tardive dyskinesia symptoms?
Tardive dyskinesia symptoms can vary from person to person but typically involve involuntary movements. These may include:
- Grimacing or facial tics
- Lip smacking or puckering
- Tongue protrusion or rapid movements
- Finger or toe tapping
- Rocking or swaying of the body
- Rapid blinking or eye movements
These movements are often rhythmic and can range from mild to severe. In some cases, TD symptoms may interfere with daily activities and quality of life.
How can tardive dyskinesia impact daily life?
The effects of TD can extend beyond physical symptoms, potentially affecting various aspects of a person’s life:
- Social interactions: Visible movements may lead to self-consciousness or social withdrawal
- Communication: Facial and tongue movements can interfere with speech
- Eating and drinking: Difficulty controlling mouth movements may affect these activities
- Employment: Severe symptoms could impact job performance or opportunities
- Emotional well-being: TD may contribute to anxiety, depression, or lowered self-esteem
Understanding these potential impacts is crucial for both patients and healthcare providers in developing comprehensive treatment plans.
What are the dangerous side effects of tardive dyskinesia?
While TD itself is not typically life-threatening, it can lead to serious complications:
- Physical injuries: Uncontrolled movements may result in falls or accidents
- Respiratory issues: In severe cases, TD affecting the diaphragm can cause breathing difficulties
- Swallowing problems: Tongue and throat movements may interfere with swallowing, increasing choking risk
- Dental problems: Constant jaw movements can lead to tooth wear or damage
- Emotional distress: Chronic symptoms may contribute to mental health issues
These potential side effects underscore the importance of early detection and proper management of TD.
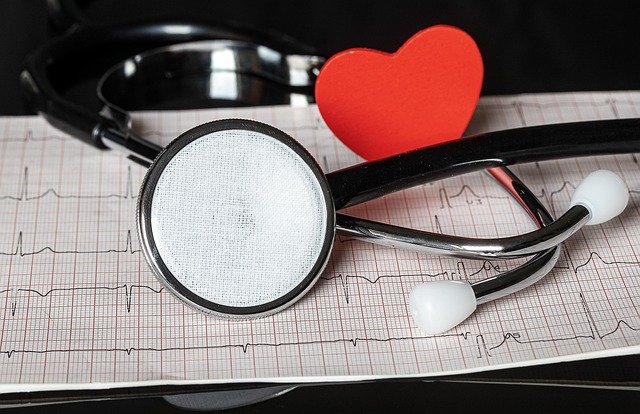
How is tardive dyskinesia diagnosed?
Diagnosing TD involves several steps:
- Medical history review: Assessing medication use, particularly antipsychotics
- Physical examination: Observing involuntary movements
- Abnormal Involuntary Movement Scale (AIMS): A standardized assessment tool
- Ruling out other conditions: Excluding other movement disorders with similar symptoms
- Monitoring: Observing symptom progression over time
Early diagnosis is key to preventing the condition from worsening and improving treatment outcomes.
What tardive dyskinesia information is crucial for patients?
- TD is often associated with long-term use of antipsychotic medications
- Symptoms can persist even after discontinuing the causative medication
- Early intervention may improve prognosis and quality of life
- Treatment options are available and continue to evolve
- Regular monitoring is essential for those at risk or diagnosed with TD
- Lifestyle modifications, such as stress reduction and exercise, may help manage symptoms
- Support groups can provide valuable resources and emotional support
What are the current treatment options for tardive dyskinesia?
Treatment for TD has advanced significantly in recent years:
- Medication adjustments: Reducing or changing the causative medication when possible
- VMAT2 inhibitors: FDA-approved drugs like valbenazine and deutetrabenazine
- Antioxidants: Vitamin E and Ginkgo biloba may offer some benefits
- Botulinum toxin injections: For localized symptoms
- Deep brain stimulation: In severe cases unresponsive to other treatments
- Supportive therapies: Physical therapy, occupational therapy, and speech therapy
The choice of treatment depends on the severity of symptoms, overall health, and individual response to therapies.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
The shared information of this article is up-to-date as of the publishing date. For more up-to-date information, please conduct your own research.