Comprehensive Guide to Lung Disease Treatment: Options and Approaches
Lung diseases affect millions of people worldwide, impacting their quality of life and overall health. Understanding the available treatment options is crucial for those diagnosed with lung conditions. This article explores various approaches to lung disease treatment, focusing on medications, therapies, and management strategies.

What are the common types of lung diseases treated?
Lung diseases encompass a wide range of conditions affecting the respiratory system. Some of the most frequently treated lung diseases include:
-
Chronic Obstructive Pulmonary Disease (COPD): This umbrella term includes emphysema and chronic bronchitis, characterized by airflow limitation and breathing difficulties.
-
Asthma: A chronic condition causing inflammation and narrowing of the airways, leading to wheezing, shortness of breath, and coughing.
-
Pneumonia: An infection that inflames the air sacs in one or both lungs, which may fill with fluid or pus.
-
Lung Cancer: Abnormal cell growth in lung tissues, often caused by smoking or exposure to harmful substances.
-
Pulmonary Fibrosis: A condition where lung tissue becomes scarred, making it difficult to breathe.
Treatment approaches vary depending on the specific lung disease and its severity.
What are the primary lung disease medications available?
Medications play a crucial role in managing lung diseases. The most common types of lung disease medications include:
-
Bronchodilators: These drugs help relax and open the airways, making breathing easier. They are commonly used for COPD and asthma.
-
Corticosteroids: These anti-inflammatory medications reduce swelling in the airways and are often prescribed for asthma and some forms of COPD.
-
Antibiotics: Used to treat bacterial lung infections, such as certain types of pneumonia.
-
Antiviral medications: Prescribed for viral lung infections, including influenza-related pneumonia.
-
Targeted therapies: Specific medications designed to treat certain types of lung cancer or other specialized lung conditions.
-
Mucolytics: These drugs help thin and loosen mucus, making it easier to cough up and clear the airways.
The choice of medication depends on the specific lung condition, its severity, and individual patient factors.
How does COPD therapy differ from other lung disease treatments?
COPD therapy options are tailored to address the unique challenges of this progressive lung disease. Key aspects of COPD treatment include:
-
Smoking cessation: This is the most crucial step in slowing COPD progression and improving overall lung health.
-
Bronchodilator therapy: Long-acting and short-acting bronchodilators are central to COPD management, helping to keep airways open.
-
Inhaled corticosteroids: Often combined with bronchodilators to reduce inflammation and prevent exacerbations.
-
Oxygen therapy: Supplemental oxygen may be prescribed for patients with severe COPD to improve oxygen levels in the blood.
-
Pulmonary rehabilitation: A comprehensive program including exercise, education, and support to improve quality of life and reduce symptoms.
-
Vaccinations: Annual flu shots and pneumococcal vaccines are recommended to prevent respiratory infections.
COPD therapy is typically long-term and focuses on symptom management and slowing disease progression, unlike treatments for acute lung conditions.
What non-medication therapies are used in lung disease treatment?
In addition to medications, several non-pharmacological approaches are essential in lung disease treatment:
-
Respiratory physiotherapy: Techniques to improve breathing and clear airways, such as postural drainage and chest percussion.
-
Oxygen therapy: Supplemental oxygen can be crucial for patients with severe lung diseases to maintain adequate blood oxygen levels.
-
Pulmonary rehabilitation programs: Comprehensive programs combining exercise, education, and support to improve lung function and quality of life.
-
Nutritional support: Proper diet and nutrition play a vital role in maintaining overall health and supporting lung function.
-
Stress management and mental health support: Coping with chronic lung disease can be challenging, and psychological support is often beneficial.
These non-medication therapies are often used in conjunction with pharmacological treatments for a holistic approach to lung disease management.
What are the latest advancements in lung disease treatment?
Recent years have seen significant progress in lung disease treatment, offering new hope for patients:
-
Targeted therapies for lung cancer: Precision medicine approaches using genetic profiling to tailor treatments to specific cancer types.
-
Biologics for severe asthma: Monoclonal antibodies targeting specific inflammatory pathways in difficult-to-treat asthma cases.
-
Bronchoscopic lung volume reduction: Minimally invasive procedures to improve lung function in emphysema patients.
-
Gene therapy: Experimental treatments targeting genetic causes of certain lung diseases, showing promise in clinical trials.
-
Artificial intelligence in diagnostics: Advanced imaging analysis to improve early detection and treatment planning for lung diseases.
These innovations are expanding treatment options and improving outcomes for many patients with lung diseases.
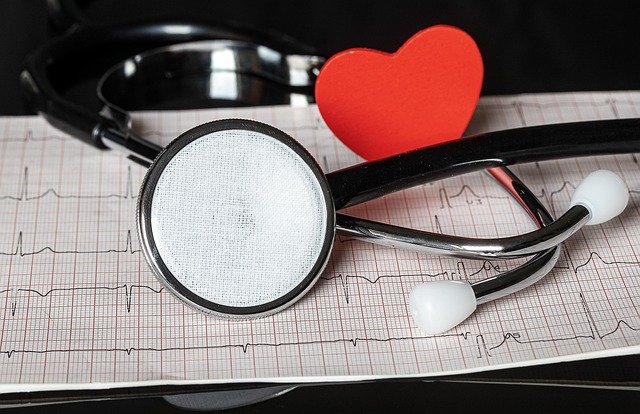
How do healthcare providers approach lung disease treatment plans?
Healthcare providers develop personalized treatment plans for lung diseases based on several factors:
-
Accurate diagnosis: Determining the specific type and severity of lung disease through various tests and examinations.
-
Patient history and lifestyle: Considering factors like smoking history, occupational exposures, and overall health status.
-
Symptom assessment: Evaluating the frequency and severity of symptoms to guide treatment intensity.
-
Lung function tests: Using spirometry and other pulmonary function tests to measure lung capacity and airflow.
-
Comorbidities: Addressing other health conditions that may impact lung disease management.
-
Patient preferences and goals: Involving patients in decision-making to ensure treatment aligns with their lifestyle and objectives.
-
Regular monitoring and adjustment: Continuously assessing treatment effectiveness and making necessary modifications.
Healthcare providers often use a stepped approach, starting with less intensive treatments and escalating as needed to achieve optimal control of lung disease symptoms and progression.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.