Comprehensive Guide to Diabetes Treatment: Options for Effective Management
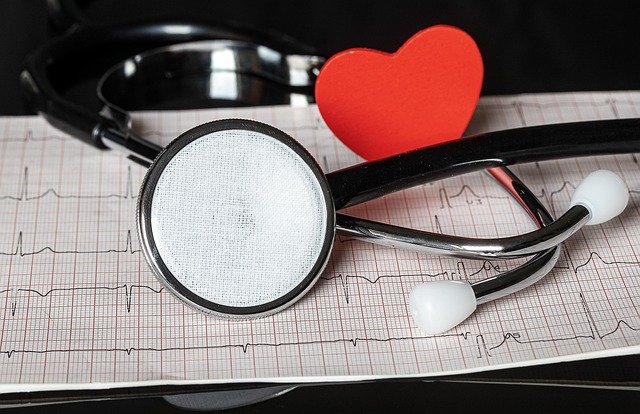
Diabetes is a chronic condition affecting millions worldwide, characterized by the body's inability to properly regulate blood sugar levels. Effective diabetes treatment is crucial for maintaining quality of life and preventing serious complications. This article explores various diabetes care options and glucose control solutions, providing a comprehensive overview of current treatment approaches.

What are the primary goals of diabetes treatment?
The main objectives of diabetes treatment are to maintain blood glucose levels within a healthy range, prevent complications, and improve overall quality of life. This is typically achieved through a combination of lifestyle changes, medication, and regular monitoring. Diabetes care aims to keep blood sugar levels as close to normal as possible without causing dangerous fluctuations. By effectively managing blood sugar, patients can reduce the risk of long-term complications such as heart disease, kidney damage, and nerve problems.
How does lifestyle modification contribute to diabetes management?
Lifestyle changes play a crucial role in diabetes treatment and are often the first line of defense. A balanced diet, regular physical activity, and weight management are fundamental components of diabetes care. Dietary modifications usually involve controlling carbohydrate intake, increasing fiber consumption, and choosing foods with a low glycemic index. Exercise helps improve insulin sensitivity and lowers blood glucose levels. For many individuals with type 2 diabetes, losing excess weight can significantly improve blood sugar control and may even lead to remission in some cases.
What medications are commonly used for diabetes treatment?
Various medications are available for managing diabetes, depending on the type of diabetes and individual patient needs. For type 1 diabetes, insulin therapy is essential and is administered through injections or an insulin pump. Type 2 diabetes treatment often begins with oral medications such as metformin, which reduces glucose production in the liver. Other classes of drugs include sulfonylureas, which stimulate insulin production, and DPP-4 inhibitors, which help the body use its own insulin more effectively. In some cases, injectable medications like GLP-1 receptor agonists may be prescribed to improve blood sugar control and aid in weight loss.
How does blood glucose monitoring factor into diabetes care?
Regular blood glucose monitoring is a critical aspect of diabetes management. It allows patients and healthcare providers to track how well the current treatment plan is working and make necessary adjustments. Traditional monitoring methods involve finger prick tests using a glucometer, while more advanced options include continuous glucose monitoring (CGM) systems. These devices provide real-time glucose readings throughout the day and night, offering valuable insights into glucose trends and helping patients make informed decisions about their diet, exercise, and medication.
What innovative glucose control solutions are emerging in diabetes care?
The field of diabetes treatment is constantly evolving, with new technologies and approaches emerging to improve glucose control and quality of life for patients. One significant advancement is the development of closed-loop insulin delivery systems, also known as artificial pancreas devices. These systems combine CGM technology with an insulin pump and advanced algorithms to automatically adjust insulin delivery based on real-time glucose levels. Other innovations include smart insulin pens that track doses and timing, and non-invasive glucose monitoring methods that are currently in development.
How do healthcare providers approach individualized diabetes treatment plans?
Diabetes care is highly individualized, as treatment needs can vary greatly from person to person. Healthcare providers typically consider factors such as the type of diabetes, age, overall health status, lifestyle, and personal preferences when developing a treatment plan. A comprehensive diabetes management strategy often involves a team approach, including endocrinologists, primary care physicians, dietitians, and diabetes educators. Regular check-ups and adjustments to the treatment plan are essential to ensure optimal glucose control and prevent complications.
| Treatment Approach | Description | Typical Cost Range (USD) |
|---|---|---|
| Oral Medications | Common first-line treatment for Type 2 diabetes | $4 - $250+ per month |
| Insulin Therapy | Essential for Type 1 diabetes, some Type 2 cases | $50 - $1000+ per month |
| CGM Systems | Continuous glucose monitoring devices | $200 - $500 for device, $300 - $600 monthly for supplies |
| Insulin Pumps | Devices for continuous insulin delivery | $4,000 - $7,000 for pump, $100 - $300 monthly for supplies |
| Diabetes Education | Classes and counseling for self-management | $50 - $200 per session |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
In conclusion, effective diabetes treatment involves a multifaceted approach combining lifestyle modifications, medication, and regular monitoring. As research advances, new glucose control solutions continue to emerge, offering hope for improved management and quality of life for those living with diabetes. By working closely with healthcare providers and staying informed about the latest diabetes care options, individuals can develop personalized strategies to effectively manage their condition and minimize the risk of complications.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.