Comprehensive Guide to Diabetes Treatment: From Medication to Lifestyle Changes
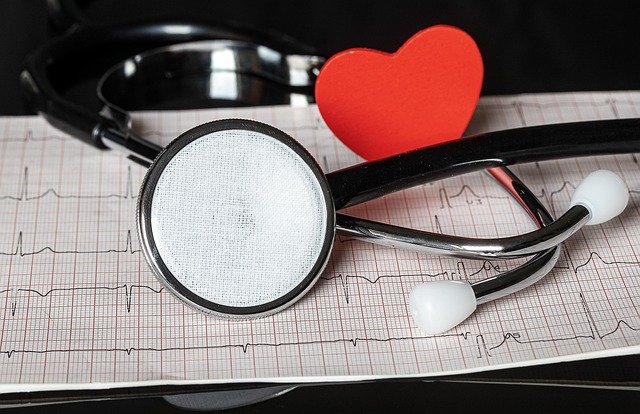
Diabetes is a chronic condition affecting millions worldwide, characterized by high blood sugar levels. Effective management is crucial to prevent complications and maintain a good quality of life. This article explores various treatment options, from medical interventions to lifestyle modifications, for people living with diabetes.
What are the main types of diabetes and their treatments?
There are two primary types of diabetes: Type 1 and Type 2. Type 1 diabetes is an autoimmune condition where the body doesn’t produce insulin, requiring lifelong insulin therapy. Type 2 diabetes, the more common form, is characterized by insulin resistance and may be managed through a combination of medication, diet, and exercise.
For Type 1 diabetes, insulin therapy is essential. This can be administered via injections or an insulin pump. Type 2 diabetes treatment often starts with lifestyle changes and may progress to oral medications or insulin if blood sugar levels remain uncontrolled.
How do oral medications help in managing diabetes?
Oral medications play a significant role in Type 2 diabetes management. These drugs work in various ways to lower blood glucose levels. Some common classes of diabetes medications include:
- Metformin: Reduces glucose production in the liver
- Sulfonylureas: Stimulate insulin production in the pancreas
- DPP-4 inhibitors: Increase insulin production and decrease glucose production
- SGLT2 inhibitors: Help the kidneys remove excess glucose through urine
The choice of medication depends on individual factors such as overall health, blood sugar levels, and potential side effects. It’s crucial to work closely with a healthcare provider to determine the most suitable medication regimen.
What role does insulin therapy play in diabetes treatment?
Insulin therapy is the cornerstone of Type 1 diabetes treatment and may also be necessary for some people with Type 2 diabetes. There are several types of insulin, including:
- Rapid-acting insulin
- Short-acting insulin
- Intermediate-acting insulin
- Long-acting insulin
Insulin can be administered through injections or an insulin pump. The dosage and timing of insulin therapy are personalized based on factors like blood sugar levels, meal times, and physical activity. Regular blood glucose monitoring is essential to adjust insulin doses effectively.
How important are diet and exercise in managing diabetes?
Diet and exercise are fundamental aspects of diabetes management for both Type 1 and Type 2 diabetes. A balanced diet helps control blood sugar levels and maintains overall health. Key dietary recommendations include:
- Focusing on whole grains, lean proteins, and healthy fats
- Limiting refined carbohydrates and sugary foods
- Monitoring portion sizes
- Staying hydrated
Regular physical activity improves insulin sensitivity, helps maintain a healthy weight, and contributes to better blood sugar control. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, along with strength training exercises.
What are some emerging treatments and technologies for diabetes management?
The field of diabetes treatment is constantly evolving, with new technologies and therapies emerging. Some exciting developments include:
- Continuous Glucose Monitoring (CGM) systems: These devices provide real-time glucose readings, allowing for more precise management.
- Artificial pancreas systems: Combining CGM with insulin pumps, these closed-loop systems automatically adjust insulin delivery based on glucose levels.
- GLP-1 receptor agonists: Injectable medications that improve blood sugar control and may aid in weight loss.
- Islet cell transplantation: A promising treatment for some people with Type 1 diabetes, involving transplanting insulin-producing cells.
These advancements offer new possibilities for more effective and personalized diabetes management, potentially improving quality of life for those living with the condition.
What are the costs associated with diabetes treatment in the United States?
The cost of diabetes treatment can vary significantly depending on the type of diabetes, treatment regimen, and insurance coverage. Here’s an overview of some common diabetes-related expenses:
| Treatment/Item | Average Annual Cost |
|---|---|
| Insulin (vials) | $2,000 - $3,000 |
| Insulin pump | $4,500 - $6,500 (one-time cost) |
| Continuous Glucose Monitor | $3,000 - $4,000 (including supplies) |
| Oral medications | $200 - $500 per medication |
| Blood glucose test strips | $600 - $1,000 |
| Doctor visits and lab tests | $1,000 - $2,000 |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
Effectively managing diabetes requires a multifaceted approach, combining medical treatments with lifestyle modifications. By working closely with healthcare providers and staying informed about the latest developments in diabetes care, individuals can develop a personalized treatment plan that helps maintain optimal blood sugar control and overall health.
The shared information of this article is up-to-date as of the publishing date. For more up-to-date information, please conduct your own research.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.