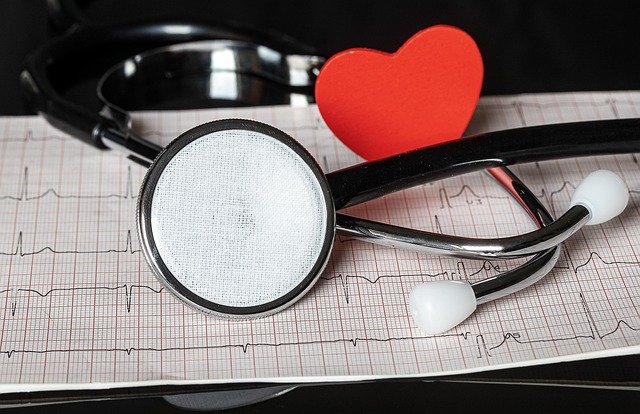
Bronchiectasis Treatment: Comprehensive Guide to Managing This Chronic Condition
Bronchiectasis is a chronic lung condition characterized by damaged and widened airways, leading to mucus buildup and recurrent infections. While there is no cure, effective treatment can significantly improve quality of life and prevent further lung damage. This article explores the various treatment options available for bronchiectasis, management strategies, and answers common questions about this condition.

What is bronchiectasis and how does it affect the lungs?
Bronchiectasis is a long-term condition where the airways in the lungs become abnormally widened and damaged. This damage leads to mucus accumulation, making it difficult to clear the airways and increasing the risk of infections. The condition can result from various causes, including severe infections, autoimmune disorders, or genetic factors. Understanding the underlying cause is crucial for determining the most effective treatment approach.
What are the primary goals of bronchiectasis treatment?
The main objectives of bronchiectasis treatment are to:
-
Manage symptoms and improve quality of life
-
Prevent further lung damage
-
Reduce the frequency and severity of flare-ups
-
Control infections
-
Maintain lung function
Treatment plans are typically tailored to individual patients based on the severity of their condition, underlying causes, and specific symptoms.
What are the most common treatment options for bronchiectasis?
Several treatment options are available for managing bronchiectasis:
-
Airway clearance techniques: These methods help remove excess mucus from the lungs, improving breathing and reducing the risk of infections. Techniques include chest physiotherapy, postural drainage, and the use of devices like flutter valves or positive expiratory pressure (PEP) devices.
-
Medications: Various medications can be prescribed to manage symptoms and prevent complications:
-
Bronchodilators to open airways
-
Inhaled corticosteroids to reduce inflammation
-
Mucolytics to thin mucus
-
Antibiotics to treat or prevent infections
-
-
Pulmonary rehabilitation: This comprehensive program includes exercise training, education, and support to improve physical and psychological well-being.
-
Oxygen therapy: For patients with low blood oxygen levels, supplemental oxygen may be necessary.
-
Surgery: In severe cases, surgical interventions like lung resection or lung transplantation may be considered.
How can patients effectively manage bronchiectasis at home?
Effective home management is crucial for controlling bronchiectasis symptoms:
-
Adhere to prescribed medications and treatments
-
Practice regular airway clearance techniques
-
Stay hydrated to help thin mucus
-
Avoid smoking and exposure to secondhand smoke
-
Get vaccinated against flu and pneumonia
-
Maintain good overall health through proper nutrition and exercise
-
Monitor symptoms and report any changes to healthcare providers promptly
Patients should work closely with their healthcare team to develop a personalized management plan that suits their specific needs and lifestyle.
What role does diet and exercise play in bronchiectasis management?
Diet and exercise play a significant role in managing bronchiectasis:
-
Balanced diet: A nutritious diet supports the immune system and overall health. Foods rich in antioxidants, vitamins, and minerals can help reduce inflammation and support lung function.
-
Hydration: Adequate fluid intake helps thin mucus, making it easier to clear from the airways.
-
Exercise: Regular physical activity improves cardiovascular health, strengthens respiratory muscles, and enhances mucus clearance. Low-impact exercises like swimming, walking, or cycling are often recommended.
-
Weight management: Maintaining a healthy weight reduces strain on the lungs and improves overall respiratory function.
-
Avoiding trigger foods: Some patients may find that certain foods increase mucus production or trigger symptoms. Identifying and avoiding these foods can help manage the condition more effectively.
What are the latest advancements in bronchiectasis treatment?
Recent advancements in bronchiectasis treatment have focused on improving patient outcomes and quality of life:
-
Targeted antibiotic therapy: The use of inhaled antibiotics delivered directly to the lungs has shown promise in reducing exacerbations and improving lung function.
-
Biologics: Research is ongoing into the use of biological therapies that target specific inflammatory pathways involved in bronchiectasis.
-
Advanced airway clearance devices: New technologies, such as high-frequency chest wall oscillation vests, offer more effective mucus clearance options.
-
Personalized medicine: Genetic testing and biomarker analysis are being explored to tailor treatments to individual patients based on their specific disease characteristics.
-
Combination therapies: Studies are investigating the effectiveness of combining different treatment modalities for improved outcomes.
What are the costs associated with bronchiectasis treatment?
Managing bronchiectasis can involve significant costs, varying based on the severity of the condition and the required treatments. Here’s an overview of potential expenses:
| Treatment Option | Provider Type | Estimated Cost Range (USD) |
|---|---|---|
| Inhaled Medications | Pharmacy | $50 - $500 per month |
| Airway Clearance Devices | Medical Supply Companies | $100 - $1,000 (one-time purchase) |
| Pulmonary Rehabilitation | Hospitals/Clinics | $1,000 - $3,000 per program |
| Oxygen Therapy | Home Health Companies | $100 - $500 per month |
| Antibiotics | Pharmacy | $10 - $200 per course |
| Specialist Visits | Pulmonologists | $100 - $500 per visit |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
It’s important to note that insurance coverage can significantly reduce out-of-pocket expenses for patients. Many insurance plans cover a portion of these costs, but coverage varies widely. Patients should consult with their insurance providers to understand their specific coverage for bronchiectasis treatments.
In conclusion, while bronchiectasis is a chronic condition, effective management can significantly improve quality of life and slow disease progression. A comprehensive approach combining medical treatments, lifestyle modifications, and regular monitoring is key to successful management. As research continues, new therapies and personalized treatment approaches offer hope for even better outcomes in the future.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
The shared information of this article is up-to-date as of the publishing date. For more up-to-date information, please conduct your own research.